Pelvic floor muscle assessment, biofeedback training, and electrical stimulation therapy have been widely popularized.
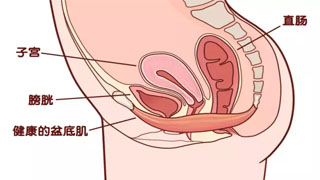
Pelvic floor muscles refer to the muscle group located at the bottom of the pelvis, whose main function is to support and control the functions of organs such as the bladder, anus, and reproductive organs. If there are problems with the pelvic floor muscles, it may lead to urinary incontinence, constipation, anal incontinence, and sexual dysfunction.
For women who are 42 days postpartum, routine pelvic floor muscle training greatly reduces the occurrence of pelvic organ prolapse and pelvic floor dysfunction diseases such as urinary incontinence. At the same time, it awakens the nerves and muscles of the pelvic floor, allowing the vagina to better return to a contracted state, thereby improving the quality, pleasure, and orgasm of sexual life.
Pelvic floor assessment is the process of evaluating the pelvic floor muscles, including anatomical, physiological, and functional assessments. The evaluation of pelvic floor muscles includes the following aspects:
Morphological assessment of pelvic floor muscles: Evaluate the thickness, symmetry, texture, and structural abnormalities of pelvic floor muscles through palpation or imaging techniques.
Functional assessment of pelvic floor muscles: Evaluate the strength, endurance, coordination, and flexibility of pelvic floor muscles through questionnaire surveys, physiological tests, and electrophysiological methods.
Neurological assessment of pelvic floor muscles: Evaluate the neural innervation and reflex of pelvic floor muscles through neuroelectrophysiological methods.
Pain assessment of pelvic floor muscles: Evaluate the degree and nature of pelvic floor muscle pain through palpation, pain questionnaire survey, and neuropathology methods.
Quality of life assessment of pelvic floor muscles: Evaluate patients' quality of life through methods such as questionnaire surveys and health-related quality of life assessments.
The exercise and rehabilitation of pelvic floor muscles are important means of treating pelvic floor dysfunction. Through professional rehabilitation treatment and self exercise, the strength and endurance of pelvic floor muscles can be enhanced, and the control ability of pelvic floor muscles can be improved, thereby improving patients' symptoms and quality of life.
Pelvic floor assessment and biofeedback training therapy involve guiding surface electromyography and measuring urethral systolic pressure, with feedback displayed as electromyography or pressure curves. By influencing the display and sound prompts, patients can have a clearer and more intuitive understanding of their pelvic floor muscle function status and participate in the treatment. Combining individualized electrical stimulation therapy can awaken and activate pelvic floor muscles, accelerate the recovery of tension and elasticity of postpartum vagina and pelvic floor muscles, and have good effects on preventing and treating pelvic floor disorders such as postpartum vaginal prolapse, relaxation, and urinary incontinence. Today, we will mainly focus on pelvic floor rehabilitation training.
Pelvic floor prevention and treatment "is not just about pelvic floor assessment and biofeedback technology. Obese women with stress urinary incontinence can lose 5% -10% of their weight and reduce the frequency of urinary incontinence by more than 50%.
What is pelvic floor muscle training (PFMT)?
Pelvic floor muscle training (PFMT) is a non pharmacological, non-surgical treatment method mainly used to treat pelvic floor muscle dysfunction, urinary incontinence and other diseases.
The pelvic floor muscles are a group of muscles that support the bladder, uterus, and rectum, and are also key muscles for controlling bowel movements and urination. With the influence of factors such as aging and childbirth, pelvic floor muscles are prone to problems such as relaxation and weakness, leading to a series of diseases. PFMT can enhance the contraction strength and endurance of pelvic floor muscles through targeted training, thereby improving pelvic floor muscle dysfunction. PFMT is a safe and effective treatment for issues such as urinary incontinence, pelvic organ prolapse, and sexual dysfunction, especially for patients who are not suitable for surgery.
The exercise method of PFMT: Continuously contract the pelvic floor muscles (anal sphincter contraction exercise) for no less than 3 seconds, relax and rest for 2-6 seconds, do it continuously for 15-30 minutes, 3 times a day; Or do it 150-200 times a day. Lasts for 3 months or longer.
PFMT, also known as Kegel training method, was initially only used as a perinatal training and teaching for expectant mothers or postpartum women to promote smooth childbirth and postpartum recovery. Later on, its use greatly expanded and it was found that this training method was very useful for diseases related to pelvic floor organ dysfunction, including urinary incontinence, defecation dysfunction, as well as various functional disorders and dissatisfaction related to female pelvic organs... you know.
The pelvic floor muscles are the bottommost group of muscles in the pelvic floor, supporting many organs such as the uterus, bladder, small intestine, rectum, etc. in women, and the contraction of pelvic floor muscles also maintains the normal function of these organs. Although the task of this muscle group is very arduous, it is very fragile. Obesity, pregnancy, childbirth, surgery, coughing, aging... are all killers of pelvic floor muscles. But we can gradually recover and strengthen the pelvic floor muscles through training to combat increased abdominal pressure.
Both vaginal and cesarean section women need pelvic floor rehabilitation after childbirth. During the process of pregnancy in October, under the action of progesterone, the pelvic floor will become relaxed; As the fetus grows up and moves downwards, the pelvic floor will also be subjected to increasing pressure, causing varying degrees of damage to the pelvic floor muscles. After delivery, as the fetus is delivered, some ligaments become loose and the elasticity of the "spring bed" deteriorates, making it impossible to fix the organs in their normal position, resulting in functional impairment. So, both vaginal and cesarean section women need to undergo pelvic floor function assessment and pelvic floor function rehabilitation treatment after delivery
Mild symptoms:
Vaginal laxity, sexual dissatisfaction, lower abdominal bloating, frequent urination, constipation
Moderate performance:
Urinary incontinence: leakage of urine when coughing, sneezing, laughing or lifting heavy objects
Pelvic organ prolapse (uterus, bladder, rectum, etc.); The genital area feels downward, the vagina feels swollen and uncomfortable, accompanied by lower abdominal distension and back pain;
Severe manifestations:
Urinary incontinence: Urinary incontinence occurs when standing
Pelvic organs detach to the outside of the vagina and often rub against it while walking, causing problems such as ulcers, suppuration, or uterine hypertrophy
Chronic pelvic pain, sexual dysfunction and other diseases
Rehabilitation training for pelvic floor muscles
During childbirth, women's pelvic floor muscles are severely damaged, so almost all women need to undergo pelvic floor muscle rehabilitation training after childbirth. So how to carry out pelvic floor muscle rehabilitation training? Today, I will introduce to you the rehabilitation training methods for pelvic floor muscles.
Pregnant women and postpartum women can practice targeted movements under the guidance of doctors or professional therapists to open the pelvis, which is beneficial for smooth delivery; Enhance muscle tension and balance of the body, improve the flexibility and agility of the entire muscle tissue; Simultaneously stimulating the glands that control hormone secretion, increasing blood circulation, and eliminating physical discomfort is also a very good rehabilitation training for pelvic floor muscles.
But pregnant women should pay attention not to bend over, hold their breath, or compress their abdomen during exercise, otherwise it is easy to harm the fetus.
Beam angle style: Sitting posture, knees bent open, hands gripping toes. Stretch your spine, place your feet against each other, and use both hands to assist in bringing your heels as close to your body as possible. Press down your knees and bring them closer to the ground. Keep your chest high and shoulders open when performing movements. Maintain 3-5 natural breaths while doing it. This posture can increase blood circulation in the lower back, abdomen, and pelvis. Practicing it daily can reduce pain during childbirth.
Chair style: Knees and feet tightly (or naturally apart), squat down halfway, as if you were about to sit on a chair. Raise your arms above your head, palms facing each other. Maintain this position and take three deep breaths. This posture can enhance body function, open the pelvis, and help with smooth childbirth.
Cat Stretching Style: Like a kitten stretching lazily, lying on the ground, stretching its spine while breathing. Place both hands and knees on the ground at four points, with the thighs and arms perpendicular to the ground; Inhale and lower your back, raise your chin, and lift your hips up; Exhale and arch your back, bringing your chin and chest closer together. It can improve the blood flow of the spine and spinal nerves, and also alleviate constipation that many pregnant women are prone to.
Leg up position: Lie on your back, slowly lift your legs together, at a 30 degree angle to the ground, hold for a while and then lift upwards, at a 60 degree angle to the ground, then hold for a while and lift upwards at a 90 degree angle to the ground. Do 2-4 sets each time, the slower the speed, the better the effect. This movement can exercise the lower abdominal muscles.
Baby style supine position: Inhale, bend your legs, embrace with both hands, exhale, and press your legs against your chest. First inhale, then exhale, and at the same time lift your head to your knees. Repeat this process three times in total. It can stretch and strengthen the neck muscles, nourish and strengthen the abdomen, eliminate abdominal dirt and turbidity, and alleviate constipation symptoms
Basic principles of postpartum pelvic floor muscle rehabilitation
The main goals and basic principles of postpartum pelvic floor muscle rehabilitation are to improve pelvic floor muscle contraction ability, prevent and treat PFD, and improve sexual quality of life. In 1940, Dr. Arnold Kegal proposed the Kegal training method to strengthen the pelvic floor muscles and reduce the occurrence of urinary incontinence. On this basis, supplemented by techniques such as biofeedback and electrical stimulation, the therapeutic effect of pelvic floor rehabilitation treatment is greatly improved.
Pelvic Floor Muscle Exercise (PFME), also known as Kegal Exercise, is a pelvic floor muscle training method.
The method is to tighten the anus for at least 3 seconds each time, and then relax. Continue for 15-30 minutes, 2-3 times a day; Or do PFME 150-200 times a day for 6-8 weeks as one course of treatment.
Pelvic floor muscle training needs to consider five aspects:
① Strength, the maximum tension that can be generated by muscle contraction;
② The ratio of speed, maximum tension, and time required to reach maximum tension;
③ Duration, the length of time that muscle contractions can last or repeat;
④ Repeatability refers to the number of times a certain tension can be repeatedly contracted;
⑤ Fatigue occurs when maintaining muscle contraction to achieve the required or expected tension.
Type I fiber training mainly focuses on strength, duration, and repeatability;
Class II fiber training mainly focuses on strength, speed, and fatigue.
Key points of rehabilitation
1. Women who have been postpartum for more than 42 days, have good uterine recovery, and are free of infection can undergo pelvic floor muscle testing in a timely manner to determine the degree of damage.
2. Using instruments to feel and learn how to contract - relax pelvic floor muscles, learn to recognize and consciously control pelvic floor muscles, and master the correct method of pelvic floor muscle contraction (avoiding abdominal muscle contraction).
3. Under the guidance of a doctor, comprehensive techniques are applied based on the individual's symptoms and the degree and type of pelvic floor muscle injury (muscle fiber damage) to provide targeted training.
4. After completing 10-15 pelvic floor exercises, one can engage in self exercise.
5. Gradual, timely, moderate, and persistent.
6. Women with urinary incontinence and pelvic organ prolapse need to use electrical stimulation and biofeedback therapy, and appropriately extend the course of treatment.
Indications and Contraindications for Postpartum Pelvic Floor Muscles
Strictly speaking, all postpartum women in the middle and late stages of pregnancy are suitable for pelvic floor muscle rehabilitation training.
For those who have the following conditions, early pelvic floor muscle rehabilitation should be carried out:
① Weakened pelvic floor muscle strength. If unable to resist resistance, with a contraction duration of ≤ 3s (pelvic floor muscle strength rating ≤ 3) or vaginal systolic pressure ≤ 30cmH2O.
② Postpartum urinary incontinence or urinary incontinence persists after childbirth.
③ Postpartum pelvic organ prolapse, such as POP-Q system score 1 or above, especially accompanied by vaginal anterior and posterior wall protrusion.
④ Pain from perineal wound scars.
⑤ Postpartum sexual quality of life declines.
⑥ Postpartum defecation abnormalities.
⑦ Postpartum urinary retention.
If there are the following situations, it is temporarily not advisable to choose pelvic floor training,
Belonging to contraindications:
① Vaginal bleeding (such as late postpartum hemorrhage, menstrual period, etc.).
② Acute inflammation of the urinary and reproductive system.
③ Individuals who require implantation of a pacemaker.
④ Patients with combined malignant pelvic organ tumors.
⑤ Dementia or unstable epileptic seizures.


