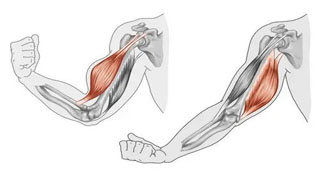
Our biceps is located in the upper arm, with the head raised at the scapula and the short head at the coracoid process of the scapula. The dorsal muscle is the triceps.
Usually, when performing upper limb reflexes, the middle finger needs to be placed on the biceps tendon, and the arm will bend when struck. The biceps muscle belongs to the skeletal muscles of the limbs, with the long head starting from the trochanter of the glenoid process of the scapula and the short head starting from the coracoid process of the scapula.
The biceps is located on the front side of the upper arm, and the entire muscle is spindle shaped. Because the head is long and short, it is called the biceps. When the arm bends, the protruding muscle between the shoulder joint and the inner side of the elbow joint is the biceps brachii. The biceps belongs to the skeletal muscles of the limbs. The long head starts from the trochanter of the glenoid fossa of the scapula, and the short head starts from the coracoid process of the scapula. The part of the humerus where the long head meets the short head is called the muscle belly.
The long head tendon of the biceps brachii originates from the tuberosity of the scapula and passes through the bone fiber channel formed by the groove between the humeral tuberosity and the transverse ligament. When the shoulder joint extends, adducts, or rotates inward, the tendon slides upwards; When the shoulder joint flexes forward, abducts, or rotates outward, it slides downward.
When the upper limb flexes the elbow outside, the long head tendon of the biceps brachii muscle is prone to wear and tear. Long term friction or excessive activity can cause congestion, edema, and thickening of the tendon sheath, resulting in acute edema or chronic inflammatory damage to the synovial layer of the tendon sheath. This can lead to obstacles in the sliding function of the long head tendon of the biceps brachii muscle within the tendon sheath, resulting in clinical symptoms known as tenosynovitis or tenosynovitis.
This disease is more common in middle-aged people over 40 years old, often caused by acute onset after trauma or strain, and is one of the common causes of shoulder pain. Its clinical manifestations mainly include shoulder pain, obvious tenderness, and limited shoulder joint movement. If left untreated, it can develop into shoulder periarthritis.
Biceps longus tendon
30% of the long head of biceps tendon (LHBT) originates from the superior glenoid tuberosity and superior labrum, 50% of LHBT originates only from the superior labrum, and the remaining 20% of LHBT originates only from the superior glenoid tuberosity.
The tendinous part of LHBT is about 9cm long and its blood supply comes from three parts: the distal end is supplied by a branch of the deep brachial artery, the proximal end is supplied by a branch of the anterior circumflex brachial artery, and the intertubercular groove is supplied by another branch of the anterior circumflex brachial artery. LHBT can be divided into two regions: the tension zone within the joint and the sliding zone within the internodal groove. The tension zone refers to normal tendon tissue, while the sliding zone is mainly composed of fibrocartilage structure with poor blood supply, and is also the main site of LHBT lesions.
The internal joint of LHBT is located between the supraspinatus tendon and the infrascapular tendon, namely within the rotator cuff gap. The coracobral ligament and superior glenohumeral ligament are stable structures of LHBT. They fold back at the entrance of the groove between nodules, forming a trochlear structure that prevents LHBT from dislocating inward. There is also a transverse ligament closure at the top of the groove between nodules, but its function is currently controversial.
At present, it is widely recognized that LHBT is mainly responsible for elbow flexion and forearm rotation, but the role of the proximal end of LHBT is still controversial, with different opinions. The results of various studies classify the functions of LHBT as compression of the humeral head, stabilization of the glenohumeral joint, and lack of any active function.
1、 Clinical manifestations
Patients with LHBT mainly present with anterior shoulder pain, which can radiate to the distal end along the muscle belly or involve the deltoid muscle. Patients generally have no obvious history of trauma. Rest can relieve the pain, but it worsens after activity. There may be nighttime pain, which is often difficult to accurately locate.
LHBT dislocation is more common in throwing athletes or patients with large rotator cuff injuries. An intra-articular clicking sound can be heard at a specific location, accompanied by pain in the front of the shoulder joint. In some patients with LHBT tendinitis, if LHBT wears away from surrounding soft tissues for a long time, dislocation or spontaneous rupture may also occur.
Acute LHBT rupture often has a history of heavy physical labor in the upper limbs. A muffled sound can be heard during strong elbow flexion, followed by pain in the front of the shoulder joint. The upper arm shows "Popeye's sign" due to the distal retraction of the muscle stump.
2、 Physical examination
The most important sign for patients with LHBT tendinitis is tenderness at the groove between nodules. After external rotation of the upper arm, the tender point should also move outward. Special inspections include speed tests and Yergason tests. However, it should be noted that the sensitivity, specificity, and accuracy of the Speed test are only 32%, 75%, and 56%, respectively; The sensitivity of the Yergason test is only 43%, the specificity is 79%, and the accuracy is 63%.
Bennett proposed the LHBT passive subluxation test: abduction of the shoulder joint by 90 °, maximum external rotation, and then passive internal rotation while retracting the shoulder joint in the forearm. If it is a subluxation patient, they may feel the instability of LHBT and accompanied by pain.
In addition, do not ignore the evaluation of the rotator cuff, especially the injury of the subscapularis muscle, which has great significance in predicting the dislocation of LHBT.
3、 Imaging examination
Routine shoulder joint frontal and lateral radiographs, as well as supraspinatus muscle exit radiographs, are taken to evaluate skeletal conditions such as acromion morphology, acromion bone spurs, and humeral head displacement. Due to the certain relationship between the morphology of the internodal groove and LHBT lesions, such as the association between shallow and flat internodal grooves and LHBT dislocation, and the association between narrow and sharp inner wall internodal grooves and LHBT tendinitis and tendon rupture, X-ray films showing the internodal groove can be taken for evaluation.
MRI can directly evaluate the morphology of LHBT and detect its dislocation or fracture. Inflammation often manifests as edema around the tendon, which is a high signal shadow on T2 weighted phase
4、 Biceps stretch
The biceps muscle is prone to tension after strength training such as bending and lifting, and pain in the front shoulder may also be caused by this reason.
Stretching using the following methods after exercise can effectively relieve muscle tension and stiffness, and enhance muscle stretching ability.
Step 1: Kneeling position, with both arms resting on the yoga mat
Step 2: Move your hips backwards, close to your heels
Step 3: Spread your arms to both sides of your body and place your palms on the ground
Step 4: Lower one shoulder and bring the chest as close to the ground as possible, then extend the arms. Step 5: Perform the same action on the other arm
In addition to the biceps, this movement can also stretch to the chest and shoulders, which is very helpful for strength training.
How to prevent and control
Biceps tendinitis
After learning the anatomy and pathogenesis of the tendon of the long head of the biceps brachii, we actually know how to prevent the occurrence of this disease. As long as we do not overuse the shoulder and avoid harmful factors, we can control the incidence rate to the lowest. However, the human body always participates in exercise and labor, so the author also reminds readers to properly maintain their long head tendons after regular exercise and labor. Common methods include:
1. Ice compress: After a long period of upper limb exercise and labor, apply ice compress to the front of the shoulder for 30 minutes. Ice compress is a convenient way to eliminate inflammation, inhibit edema and adhesion.
2. Shrugging: Slowly and rhythmically shrugging for 5 minutes each time will not increase the damage to the long head tendon, but can also relax the soft tissues of the shoulder and prevent adhesions.
What should I do if I accidentally get biceps tendinitis? The treatment recommendations are as follows:
Conservative treatment:
Firstly, it is necessary to reduce or even stop exercise and labor, increase the frequency of ice packs, and apply ice packs 3-4 times a day. Avoid hot packs during the acute phase as they may increase adhesion.
2. Take nonsteroidal anti-inflammatory drugs (Nsaids) orally appropriately, such as naproxen, indomethacin, diclofenac sodium, celecoxib, aripiprazole, etoposide, etc. Choose one of them to take after meals. For those with digestive ulcers, use with caution or use as an adjuvant gastroprotective medication.
3. Use muscle relaxants: Chlorzoxazone or Iprison, either alone or in combination with nonsteroidal anti-inflammatory drugs.
4. Use of topical anti-inflammatory drugs: such as flurbiprofen gel paste or voltarin ointment, especially for patients with gastrointestinal ulcer who cannot tolerate oral drugs.
Intermediate frequency therapy and shock wave therapy are commonly used physical therapy methods.
6. For patients with recurrent symptoms, severe conditions, intolerance to medication, and allergies to external medications, or those who require rapid recovery, local closure treatment of the internodal groove can be performed. Reasonable closure treatment is a powerful tool for treating long head tendinitis, but it is best performed by experienced doctors or doctors engaged in shoulder joint surgery, otherwise tendon rupture after injection may occur.
The above are relatively common treatment methods. If treatment is still ineffective after 2-3 weeks, further uric acid and rheumatoid factor testing should be performed to rule out the presence of gout or rheumatoid arthritis, or shoulder joint MRI examination should be performed to rule out severe wear, degeneration, thickening, synovitis, and tear at the starting point of the long head tendon, and to determine whether it is combined with acromion impingement syndrome and rotator cuff injury.
Surgical treatment:
Surgical treatment is also a treatment method for long head tendinitis, generally used for cases where conservative treatment has failed or is combined with acromion impingement syndrome and rotator cuff injury, as well as injuries to the upper labrum of the scapula involving the origin of the long head tendon (SLAP injury). Surgical methods include cleaning of the long head tendon, cutting of the long head tendon, and re fixation after cutting of the long head tendon, all of which can be performed under minimally invasive arthroscopy.


