Plantar fasciitis (PF) is one of the most common causes of foot pain. Research estimates that PF accounts for "11% to 15% of all foot symptoms in adults that require professional care. More specifically, Koteswaran et al. PF was found to be the cause of 80% of all reported cases of heel pain.
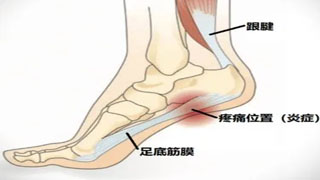
PF is usually defined as "inflammation and swelling of the plantar fascia, which is a dense tissue band that runs through the sole from the back of the heel. It is usually caused by overuse, poor natural mechanics, overweight, exercise, or inappropriate shoes, and often occurs in people between the ages of forty and sixty.
What is plantar fasciitis?
Plantar fasciitis is one of the most common diseases that cause heel pain. It involves inflammation of the plantar fascia - a tough fibrous tissue band that extends along the sole of the foot. The plantar fascia is attached to the heel bone (calcaneus) and the base of the toes. It helps to support the arch of the foot and plays an important role in normal foot mechanics during walking.
When you place weight on your feet (such as under pressure), the tension or pressure on the plantar fascia increases. When you push your feet and toes hard, the tension also increases. Both of these exercises occur during normal walking or running. If overused or over time, the fascia may lose some elasticity or resilience and may be stimulated by daily activities.
What causes plantar fasciitis?
Fascial inflammation and pain may be caused by the following reasons:
Increased activity level (such as starting a walking or running plan)
The structure or shape of the feet
The surface on which you stand, walk, or run
The type of shoes you are wearing
The weight you bear
Less commonly, plantar fasciitis may be caused by other diseases such as lupus or rheumatoid arthritis.
What are the symptoms of plantar fasciitis?
The pain of plantar fasciitis usually gradually intensifies and is usually felt near the heel. Sometimes the pain may be sudden, occurring after missing a step or jumping from a height. The pain is often most severe when you wake up in the morning or during other periods of inactivity. That's why it's called the first step pain. After daytime activities or warm-up exercises, the degree of discomfort may sometimes decrease, but after prolonged or intense activity, the degree of discomfort may worsen. When barefoot or wearing shoes with extremely low support, the pain may also be more severe.
Diagnosis of Plantar Fasciitis
Plantar fasciitis is one of the various diseases that cause heel pain.
Other possible reasons include:
Compression of nerves in the feet or back
Calcaneal stress fracture
The fat tissue pad beneath the heel is missing
Based on medical history and doctor's examination, plantar fasciitis can be distinguished from these and other conditions.
Heel bone spurs are often mistakenly believed to be the sole cause of heel pain. Although they are common, they are simply a response of the bones to the traction or tension of the plantar fascia and other foot muscles. Heel bone spurs usually do not cause any pain. It is rare for a truly enlarged and problematic bone spur to require surgery.
Treatment of Plantar Fasciitis
Generally speaking, the longer the symptoms appear and the more severe the pain, the longer the treatment time required. In addition, high demand athletes, such as cross-country runners or marathon runners, may require longer treatment courses.
The treatment plan for plantar fasciitis includes:
Stretching exercises and physical therapy
Stretching exercise is one of the best methods for treating plantar fasciitis. Stretching should be focused on the plantar fascia and Achilles tendon. A physical therapist can show you stretching exercises, which you can repeat several times a day at home. In addition to stretching exercises, these exercises can also strengthen the calf muscles and help stabilize the ankle.
Ice compress and medication treatment
Applying ice to the sore areas of the soles of the feet multiple times a day may help alleviate pain and inflammation. Your doctor may also recommend nonsteroidal anti-inflammatory drugs.
Rest, activity adjustment, and orthotics
During the healing of the plantar fascia, it helps to reduce the weight and pressure on the foot (at least partially). Your doctor may recommend the following combinations:
Replace with a more shock-absorbing sports surface
Change to shoes with arch support or try using heel cups or other orthotics to cushion the heel
Apply sports tape to the feet to support muscles and ligaments
Wear a nighttime splint to continue stretching your feet while sleeping
Reduce the distance and duration of walking or running
Switch from jumping or running to swimming or cycling
Shock wave therapy
This therapy is based on delivering low-energy or high-energy shock waves to specific areas. Shock waves can cause minor injuries, triggering the body's healing response. This process is believed to help promote the healing of the plantar fascia.
steroid injection
In most cases, plantar fasciitis will improve after several months of stretching. If symptoms persist after two months of treatment, doctors may recommend injecting steroids to alleviate inflammation.
As a supplement to ice and hot compresses, several types of physical therapies have also been used to treat pulmonary fibrosis. Some of them include "massage, activity, treatment with ultrasound and patching", as well as stretching and strengthening the muscles and ligaments around the feet 1,3,5. In a 2019 study, Thong On et al. compared the effects of reinforcement and stretching exercise programs on reducing pain and improving gait in PF patients. Strength training includes toe bending exercises, ankle eversion/inversion exercises, and heel elevation exercises; The stretching plan involves stretching the gastrocnemius and soleus muscles, as well as the plantar fascia.
Although the conclusion drawn is that both strengthening and stretching exercise programs can alleviate pain and improve gait performance in PF patients within 3 months, careful examination of the results shows that "heel lifting exercises also bring additional benefits," according to Thong On et al. It increased the strength of the ankle dorsiflexor and plantar flexor muscles, [and] expanded the range of motion and stretched the calf and Achilles tendon, "he added
Physical therapists may also recommend active release techniques (ART)
——A motion based massage technique used to address soft tissue issues in the body, including fascia, muscles, nerves, and ligaments, as well as myofascial release technique (MFR) - a low load, long-term stretching technique that typically involves applying slow, sustained pressure directly or indirectly to the restricted fascia layer to help treat PF. Pragasame et al. compared the effectiveness of ART and MFR in PF patients in a 2019 study. They determined that both ART and MFR can effectively alleviate pain and improve functional performance in PF patients. In addition, although both techniques have similar improvements in functional performance, their research results indicate that ART is more effective than MFR in reducing pain.
Other methods for treating PF include mechanical therapy (MT) selection (i.e. insoles, ankle orthotics, tapes, and shoes), corticosteroid injection, low-intensity laser therapy, ultrasound therapy, and in some extreme cases (less than 5%), surgery. The study conducted by Schuitema et al. focused on the therapeutic effect of MT on PF patients and found that "contour full-length insoles are more effective in relieving PF related symptoms than heel cups", and pointed out that "tape is an effective method". Short term treatment Some studies also list corticosteroid injections as short-term benefits in certain situations. Buchbinder et al. stated in an article published in the New England Journal of Medicine that "a reasonable intervention approach for PF patients is to start with patient-centered, low-risk, and lowest cost interventions, such as regular stretching of calf muscles and plantar fascia, avoiding wearing flat shoes and walking barefoot, using over-the-counter arch support and heel pads, and limiting prolonged physical activity. Continuing to affirm, "More than 80% of patients will have their symptoms disappear within a year


